 It comes from nowhere, like the proverbial thief in the night sneaking up silently behind you to steal your life. Perhaps a better analogy is an earthquake, but only if you were trapped in the rubble, unable to climb out. It hits unexpectedly and leaves you to figure out how to survive. In a split second, everything changes. EVERYTHING changes the moment you’re told you have cancer.
It comes from nowhere, like the proverbial thief in the night sneaking up silently behind you to steal your life. Perhaps a better analogy is an earthquake, but only if you were trapped in the rubble, unable to climb out. It hits unexpectedly and leaves you to figure out how to survive. In a split second, everything changes. EVERYTHING changes the moment you’re told you have cancer.
Once the shock wears off, if you’re like me, you get to work. In my case, the barrage of tests was supplemented with an avalanche of articles about each new term that was uttered by any of the many doctors I’d seen. Finally, I was left to figure out what to do about these two tumors in my left lung and their aftermath.
Desite the support of an incredibly loving husband whose reading and research dwarfed mine, my obviously scared but very stoic 17-year old daughter, and the kind words, thoughts and prayers of friends – both in real life and of the radio and virtual sort– I’ve never felt so alone in my life.
The tumors were growing in my body, I was the one who had most of my left lung surgically removed and now must decide whether or not to subject my body to toxic chemotherapy. If the cancer didn’t kill me, the stress from the worry and the enormity of this decision, or the chemo itself probably would.
Back to the question: To Chemo or Not?
Before I could answer that, I needed more information. Last week, we went for a really good second opinion consultation with Dr. Luis Raez at Memorial Cancer Institute in Pembroke Pines, FL. His analysis of my situation was mostly in sync with what we were told by my oncologist, Dr. Raja Mudad from UM/ Sylvester. They both believe what the pathology said
As the tumors differ histologically, and the smaller lesion also has a lepidic component, they are best classified as two distinct primaries (synchronous tumors).
That almost sounds definitive, but not quite. Because it isn’t! The tumors are “best classified” that way, but the doctors can’t, and won’t say any of that with 100% certainty.
We do know for sure that this was NSCLC (Non Small Cell Lung Cancer), which accounts for about 85% of all lung cancer. The type is adenocarcinoma, the most common form. My case is not at all rare, but it is quite unusual for a few reasons:
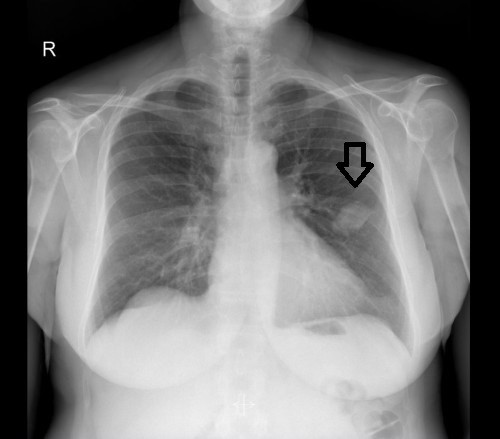
- I am the luckiest person on the planet because we caught it so early. If not for getting so upset after a really shitty day that I had a suspected heart attack (which turned out not to be a heart attack), I’d probably still be walking around with cancer growing in my lung. The x-ray of my heart clearly showed a mass on my lung that otherwise could have continue growing undetected for years.
- I’m young! I know, stop laughing. I’ll turn 57 in November but, in the world of lung cancer, I’m a baby. Unfortunately, most people don’t discover they have lung cancer until it’s had much more time to grow and metastasize. Most lung cancer patients are in their 70’s and their disease is much more advanced than mine.
- And, if we are to believe what the pathology tells us, these are two separate and distinct primary cancers, growing in separate lobes of my left lung, at the same time. Because of this oddity, I am not eligible for any clinical trials or studies. They only want common cases of cancer, not unusual ones like mine.
I like and cautiously trust these two doctors, whose advice matched what we had been told all along: that if the two tumors in my left lung were separate and distinct tumors – two primary cancers – that chemo would be not necessary because we caught them early enough and were able to surgically remove them. This is the only time doctors ever use the word “CURE” regarding lung cancer.
What About Molecular Testing?
There’s one other element to all of this. The tissue was sent for molecular testing. The first three of four results came back negative two weeks ago, but we were still waiting for the results of the test for the EGFR Gene Mutation Protein Effect Prediction when I went for the second opinion consult with Dr. Raez. At that time, he mentioned to us a national study for a drug that directly deals with that mutation. He said that if the test came back positive, we could return to the Memorial Cancer Institute, and he’d put me on the pill. Seemed simple enough. Or not.
It turns out that my very common cancer would make me a good candidate for this study. But because I had two of them, I’m ineligible for any clinical trials. Period. It seems the drug companies who fund the trials only want the most common, ordinary cancer scenarios, and I’m just too damned unusual.
So here we are. Tuesday marks five weeks since my surgery, just a week shy of three months since that fateful Thursday afternoon in early July when I thought I was having a heart attack – an event that led to the chest x-ray that very clearly showed a mass on my left lung.
I’ve long battled depression – something I’ve spoken openly about on my show, as I am doing with cancer, because I believe we’re stronger together (sorry about that), and that these diseases often make us feel so alone. I want to share all I’ve learned and experienced as a way to help others who also riding on this nightmarish roller coaster of life.
Where does this leave us?
I asked the doctor about the correct terminology. I didn’t think I was in remission –and he told me that I’m not. That’s a term usually reserved for those who’ve fought the disease via chemo, radiation and/or other modes of treatment and whose scans and tests don’t find any signs of the cancer still present.
“But obviously you can’t say that I’m cured,” I countered. “No,” he answered. “You are cancer-free,” he told me.
I have decided that I will not have chemo. That was the advice I received from the two oncologists (in as noncommittal ways as possible). What follows is a future where I’ll be watched very closely.
I’ll be scanned every three months for at least the next two years. Then, perhaps, every six months. We’ll also keep a close eye on the spot on my right lung (now very, very tiny), and I have another MRI scheduled to check in on the thing on my brain (that every doctor I’ve seen believes is a benign meningioma).
If the constant monitoring for five years shows no signs of a recurrence, then they’ll actually be able to say that my lung cancer was cured by early detection followed by surgery.
If you missed this journey from the beginning, it’s detailed in my Fuck Cancer blog here.
I’ll have much more to share in the coming months, including about my experience at the hospital after surgery, how hindsight may be 20/20 but is also upsetting, and more.
On top of that, I think it’s time to start working again. We have a presidential election coming up in a month!
There’s a lot to do before I go back on the air. We’ll start slowly… I hope to bring back the “What’s News?” segments as early as Tuesday! And I hope to be back on the air as soon as next week, starting out with a one-hour show, Tuesday through Friday afternoons from 3-4pm ET/noon-2pm PT on the Progressive Voices Network and here on our listen live page at nicolesandler.com and take it from there.
You’ll have to tell me what I missed! I think we have a lot to talk about.
In the meantime, you don’t have to be a smoker to get lung cancer. But if you smoke, your chances of getting it are much higher. You might be eligible for a free low-dose CT scan lung cancer screen. Please click here, get the information and get checked.




Actually, the term he should have used is “NED” (no evidence of disease). I know that anecdote is not data, but my mother had adenocarcinoma of the lung also (non-small cell). It was caught very early — by accident, as yours was. She too had surgery and lived another 20 years. She would probably still be here but she took up smoking again after the surgery and died of complications from COPD at 85. So much room to be optimistic.
Fantastic! Cancer-free! Looking forward to hearing you on the air again (the What’s News was terrific), but be sure to take good care of yourself.
As long as we still have to walk through huddles of people outside business doors puffing away, we are all smokers. I someone needs the nicotine, they should just use a patch. Smoke stays with the clothes for a while and as the person moves about or sits down, the smoke can still be carried by them for up to fifteen minutes. Does the meningioma have any relation to restless legs?
Heart-warming news in this crisis, Nicole; especially in light of what could have been without the early diagnosis. I know it is still a long and lonely road out there for cancer survivors, but if you can avoid chemo that is SO fantastic. It is a nasty and long-lived cure that no one should have to suffer for good quality of life.
➺ Warm hugs from SherBear and continued strength to you, Allison and David. ☯ Not a bit surprised he’s been right there by your side.
♥ Be well, and the news that you will be back on air part-time soon is extraordinary. You’re one strong survivor, woman. And you are by no means alone. ♥
So glad to hear that you have made your decision.
It sounds like a good one! The words “Cancer-Free” are wonderful.
Monitoring every 3 months is a good thing!
I’m glad to hear that you are coming back on the air.
Even though we all miss your voice, take it easy and don’t overtax yourself.
After all that you have been through, the election seems unimportant!
After all, good health and people who love us are what life is all about.
Take care & welcome back!!
Nicole, this is Elaine, I’ve also been known as SoloPocono online. I left the long msg on
your FB post before reading this. First, sorry for such a long post. It’s really late and I tend to get overly wordy when tired. I’m also getting SO tired of seeing friends, family and acquaintances diagnosed with cancer, some in late stages. I was recently told about several children, both with late-stage children’s cancers-and have just gotten very upset about these poor kids, robbed of their childhoods-and soon their lives; having to suffer through years of horrifying chemo…and their poor parents and siblings and the pain they’re dealing with. I don’t know these children or their families; but we share this horrible monster, that kills millions every day. What a terrible club to belong to.
As I said in my FB comment; it sickens me to know what is going on the the pharmaceutical industry. Do I know absolutely that a cure or a vaccine is being suppressed? No. But what I DO know is that the Govt has cut back on research money to organizations that DO, (primarily) operate their research without the concerns for profit involved. I DO know that these non-profit groups and hospitals like St Jude’s have had much less charitable donations since 2008. And I DO know that pharmaceutical companies-especially the older, major companies who actually have the money and connections to get new medications through the expensive and overly complicated process of testing, aren’t putting as much effort into this for these possible life-saving drugs as they could. In fact some things I’ve found out recently, (the big companies buying out desperate small companies who’ve gone broke doing the legwork on some VERY promising drugs-buy the rights to these drugs, then get put on the back burner, for no explainable reason. I know of 2 specifically, within the past 1 1/2yrs), have made me so angry I spent months writing letters and making calls trying to find out WHY it appears that promising drugs and treatments are being squashed-or at the very least, delayed. The only response I got-or actually my friend in the industry got-was that the 7 years of intensive testing weren’t enough to convince this major company to spend the tens of millions it costs to get it through those last hurdles. They’re going to do their own testing-starting next summer. They’ve had the drug for a YEAR.
Welcome to the pharmaceutical industry.
The “GOOD” news? There’s some small biotech companies, run by “kids” (under 40s :), getting some investment money from-lets just say “unusual, unlikely” investors, who are trying their damnedest to do their research and go through the process away from the “sharks”-if that makes sense. Some of these kids do come from “family money”, but groups of them are banding together to avoid becoming a part of the “Profit before Patients” Big Pharma system. Some are doing incredible research with the new iRNA & CRISPR technologies and are working alongside scientists at MIT, Stanford, Oxford and other Universities. Do the Sharks sometimes come out to the media talking about how this work is “wishful thinking” and “pie in the sky ridiculous”? Yep!! Can’t imagine WHY!! They’re actually trying to force regulations on some small companies-you know, for “safety”. And considering the revolving door in our FDA, right NOW, the chances of getting new technology by these small companies-at least here in the US-through the process is about nil. BUT, I know several companies have moved overseas, or even up to Canada, to try and thwart the efforts of the giants. I know one company with a vaccine-that’s been shown to have 96-98% efficacy against prostate cancer (up to at LEAST 7 years, little to no side effects!), moved just its corporate offices to the Bahamas-so far they’ve gotten approval in India and I’ll have to check for the latest in Europe, (I haven’t checked or talked to my brother in a few months-he knows the CEO). They’re doing everything they can to get through the US process without merging with one of the Sharks (who’ve been making offers for a year) but until they can get some money coming in from overseas sales, the cost here is just too prohibitive.
Things ARE changing, but it’s going to take some major changes from the top! And time. Time those kids-and millions more, don’t have.
Sorry about the novel-I’ll get off my soapbox now. I got SO involved with this last year to the beginning of this year; like with politics, I had to back off for awhile. All the above got me involved with something else, which as a diehard progressive, caused a BIT of conscious-wrestling for awhile. But being housebound, often bed-bound, in a wheelchair (“part-time” 😉 I’m still fighting it :), dialysis and my vision failing (anything more than 3ft is blurry); I’m extremely limited in ways to try and make money. AND, this whole experience yanked me out of a long depression, learning a whole new skill-lol, and scaring the shit out of me learning about the world’s financial systems! Speaking of which…I’ve got some research to do before I get some sleep!
Anyways-as far as YOU; CONGRATS on at least shutting the monster down for now-hopefully for GOOD!! I think we’re both “blessed” by the cosmos, in the sense we caught it early enough! My Doc (that agreed to take me despite not accepting Medicaid! Those 20yrs in medicine resulted in some lifelong friendships, one of whom knew him), said that just one more month-it would have cut off a major vessel! Thankfully you didn’t have to deal with the poison-and I’ll send plenty of positive thoughts and hope-that you never will! Every time I read the word “chemo”- I can taste and smell that horrible acetone! I’m currently just taking some supplements, (I took myself off almost all my allopathic meds! Thanks to Mike Papantonio, I came off my last “minor” stomach med last month!), doing my yoga and practicing daily mediation. I’ve even got both of my 90-something parents taking turmeric (they’re both Ca survivors), and my Dad offered to testify when they were trying to get medical cannabis down there! (He’s in Tally-my “home”). I’m going to be moving from Pa next Spring-either Orlando or Denver-where my Son is. My younger daughter is an RN-Paramedic in Orlando and REALLY wants me there-we’ll see!
Take it easy and I’ll try and tune-in for your upcoming shows! My kids were really active in Bernie’s campaign, but my daughters are now with Hillary, my Son and I (IF I’m even allowed to vote again this year-I wasn’t in 2012-14. The joys of living in tiny teabagger-town) are sticking with Jill. My conscious just can’t take voting for Hillary…
Here’s to knocking the monster out for the count!! ??
Elaine! It’s been a LONG time. I remember you from the Air America days (I remember SoloPocono!). Thanks for the info.. And for checking in!! xo
Glad to see you mentioned turmeric as one of many ways to combat nasty disease and I still want to mention the benefits of alkalizing the body. A little lemon + baking soda is one of nature’s simple means to prevent. Here is a site with great and simple info-
http://naturalmentor.com/baking-soda-and-lemon-juice-combo-eradicates-cancer-cells/
Yea! We will be patient because you need to feel better.