My best medicine
I had planned on posting this a few days ago. Unfortunately, the painkiller haze, the pain itself, minor (and some major) meltdowns, and my need to sleep and rest delayed it slightly.
I also want to write posts on the surgery itself (that’ll be quick as I was out for the entire thing, but there are a few notes to pass along) and my hospital stay (avoid the University of Miami Hospital like the Plague!!), so those will be coming soon. And I’ll keep you posted on the next part of the cancer fighting portion of my life as my recuperative hiatus from my radio show continues.
Up next, the Recuperation Roller Coaster….
But first, I’ve heard from a few readers/listeners that you like to hear about the technical side of all of this. You were fascinated by the YouTube videos I posted of the robotic surgery that I had and the alternative, the open thoracotomy video that I didn’t embed, but posted a link to instead.
I employ that technique a bit further down in this post. I’m sharing my one and only nude photo – so hackers can look elsewhere. Seriously, there’s nothing sexy about my nude photo. It’s a picture of the left side of my body showing the surgical incisions. But you’ll have to read on first…
Ups and Downs
I hate roller coasters. Aside from the fact that I’m terrified by heights, the huge drops make me nauseous. I don’t understand their appeal. Too bad for me, I’m currently on the most unpleasant of life’s roller coasters and I don’t like this one either, but I can’t just get off. I’ll have to ride it until the end.
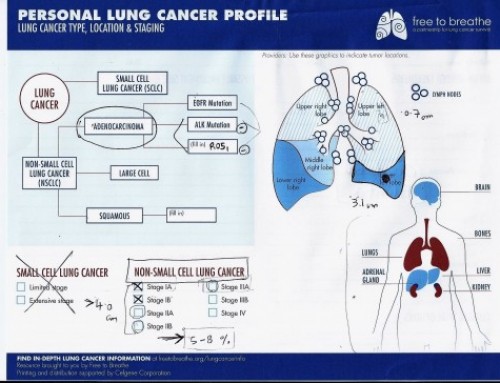
This ride actually began about two months ago when we learned, purely by accident, that I have lung cancer. In the midst of the battery of tests that followed, the CT scan turned up a second tumor. The first, primary tumor was in the left lower lobe. The second one was detected in the left upper lobe.
The post-surgical experience so far has been a series of contradictions. We’d been told all along that since we caught the cancer so early, surgical removal of it meant “cure” – the only time they ever use that C word in connection with cancer.
Then, we learned about the second tumor, but the same optimistic tone ensued. “If they are two separate, primary tumors, then it’s still Stage 1 and removing them by surgery would cure me. No chemo would be necessary.
We were told that by every doctor we saw. That accidental discovery of the mass in my lung was a life saver! We found it early enough that I can emerge from surgery cured and cancer-free!
I had surgery just over two weeks ago. I’ve been fairly quiet since then as recuperation takes a lot of energy, and my emotions have been all over the place. I posted a few updates, but mostly I’d been counting the days until the pathology report came in so I’d know what I’m facing.
My surgeon, Dr. Dao Nguyen at Sylvester Cancer Center in Miami, showed me why he is not known for his great bedside manner. But I was impressed with his background, training and patient reviews so choosing him was almost a no-brainer.
We had our post-surgical follow-up appointment last Thursday, Sept 8. Although the pathology was due by Tuesday, Sept 6, Dr. Nguyen told us it wasn’t in yet! Ugh! He did say that we’d need to meet with my oncologist, as that’s who we’ll work with to determine the course of treatment. He said he’d see me in six months for our next follow-up.
Alrighty then.
Not being a very patient person, the next afternoon I texted Dr. Nguyen to ask if the pathology had come in yet! He said he’d let me know.
Then on Monday morning, after still not hearing from him, I called the Pathology department at UM Hospital directly to ask when I could expect the results. The person who answered told me that they had sent the tissue for further tests, and it would be another 10-15 days!
After I spent a while simmering, my husband awoke and asked, “What about the preliminary report?” Duh. So I called back. The person who answered this time told me that the report was there and ready. Huh?
Rather than calling the surgeon again (remember he said he’d let me know), I texted his Nurse Practitioner, Joy Stephens- McDonnough (she was the one really good part of the surgical experience). She told me she’d check with him. A few hours later, she responded, telling me to call the doctor. I did and his office then sent me the report.
That afternoon, I had an appointment with an oncologist at Holy Cross. If you read back to the beginning of these posts, you’ll notice that I backed in to the Holy Cross Bienes Cancer Center.
A quick recap
The lung mass was detected on a chest x-ray ordered due to a suspected heart attack that ultimately wasn’t a heart attack. I already had an appointment set for the following Wednesday with a pulmonologist at Holy Cross for my sleep issues. As the pulmonologist is the doctor that also deals with all things lung-related, the focus of that appointment was the lung mass. He ordered a PET-CT scan and we were off and running.
When the CT scan showed that it was a tumor, the pulmonologist referred me to the lung cancer oncologists. Dr. Drew, the lead oncologist was on vacation, so we made an appointment with Dr. Dammrich who coordinated all the tests, scans, etc and ultimately delivered the final diagnosis, with surgery as the recommended treatment.
Now, post-surgery, Dr. Dammrich is on vacation, so on Tuesday (9/13) we met with Dr. Drew. At Holy Cross and all the other cancer centers we’ve consulted with, the doctors in the department work as a group, reviewing the cases together to come up with diagnoses and treatment plans. When he first looked at the pathology report, Dr. Drew was all smiles and upbeat. He was about to say something along the lines of “you’re good to go” when my husband David said he had a few questions from reading the report.
David pointed out that the report said the smaller tumor (LUL) was “Adenocarcinoma, acinar predominant, moderately differentiated,” and the primary tumor (LLL) was “Adenocarcinoma, acinar predominant, poorly differentiated,” at which time Dr. Drew’s upbeat demeanor instantly changed. He asked where we saw that.
I opened my copy of the pathology report and showed it to him. It seemed like all the color drained from the doctor’s face before he told us, “Forget everything I just said.”
I honestly can’t remember much of what he said after that, other than that he was wrong, he believed the pathology report was wrong where it says that these “are best classified as two distinct primaries (synchronous tumors),” and he now believed I would need chemo too.
I’m sure I asked him why, but couldn’t tell you what he said.
I do know that the lung cancer team there meets today and will review my case. My next appointment with Dr. Dammrich is Tuesday 9/20, at which time we’ll find out (hopefully) if I’ve qualified for a clinical trial there involving immunotherapy. If I don’t get into that one, there’s a second trial testing CMET (something I couldn’t possibly explain but has to do with inhibiting the growth of cancer cells) that I might qualify for.
Hopefully, I’ll be able to provide much more information on clinical trials soon. If I am, it’ll be because I’ve been accepted into one. These clinical trials are wonderful if you can qualify. Although you’re not guaranteed to get the experimental drugs even if you are accepted into the trial, everyone gets the standard of care treatment. In my case, the two drugs are called Cisplatin and Alimta, given every three weeks for four cycles. Once the chemo is completed, then you might possibly get the experimental drugs. Regardless, you get the chemo, and at no cost to you or your insurance company.
I also have another consult scheduled with an oncologist affiliated with the UM/Sylvester Cancer Center on Thursday. The lung cancer group there, including my surgeon, is also reviewing my case in their conference today.
**Update** This afternoon, as I was getting ready to post this, my phone rang. It was my surgeon, and the case conference had just ended. Sadly, I really couldn’t ask him a question. He had called to tell me that they had confirmed that I had two separate and distinct cancers. When I asked if he still thought I needed chemo, he told me that’s a decision I’ll make with the oncologist. He asked if I wanted to schedule a consult with the lead oncologist at Sylvester who was present at the conference, so he’s as well-versed as possible on my case. (He also mentioned that this oncologist, Dr. Mudad actually trained Dr. Dammrich. It’s a small oncological world after all.)
By this time next week, I’m pretty sure we’ll have decided on a course of treatment and will be ready to move on to the next phase of this nightmare.
Two Weeks Home Tomorrow
Tomorrow marks two weeks since I was released from the University of Miami Torture Chamber Hospital. I’ll have a bit more about that soon. In the meantime, here’s a snapshot of what I’ve been dealing with.

That’s my white board on which I keep track of what phone calls I’ll have to make, what referrals to get, what medications to take and what time I last took them and are due to take them next.
I won’t embed this graphic picture because 1) many people do not want to see photos of my incisions 2) it’s kind of gross and 3) it’s a semi-nude photo (though nothing even slightly titillating is visible, but still….). After that warning, if you’d like to see it, just click here.
If you chose to look at the incisions, please know I’ll explain all in a post about the surgery, coming as soon as I can knock it out. Just know they look so much better now than they did just about a week ago when David took those oh-so-not-sexy nudes!
Why I’m Sharing So Much
I’m writing these updates, albeit much less frequently than I had planned due to a variety of reasons, because I know that I’m not alone.
In 2016, there will be an estimated 1,685,210 new cases of cancer diagnosed. In 2016, it’s estimated that 595,690 people will die from cancer.
That same source tells us that this year, there will be 224,390 new cases of Lung and Bronchus Cancer diagnosed, and some 158,000 will die from it.
Looking at those numbers, I realized that “I’m not alone” is a huge understatement.
If I can help one more person navigate these waters, then sharing every detail of my experience is warranted.
If you want to receive these updates via email, please subscribe to my WTMI (WAAAY too much information) Fuck Cancer mailing list here.
As I’m feeling better and weaned off the pain meds a bit more, I’ll post more. There’s a wealth of information to share – the most surreal being the hospital bills starting to pour in which confirm my contention that the for profit health insurance industry is government-sanctioned extortion.
If you’d like to help financially, I’m like a squirrel foraging for winter, and have set up a fundraiser at YouCaring.com/nicolesandlercancer. As Jon Snow tells us, “Winter is coming.” (Apologies to all who are not Game of Thrones fans.) Although we’ve met our annual out-of-pocket maximum so the insurance company is paying 100% of the charges (with some fighting on our part), January will soon arrive. With the new year will come a new insurance company and new policy (UHC is pulling out of the exchanges, but honestly, I’d drop them if they didn’t drop us first), and new deductibles and co-pays.
Sadly, my relationship with cancer will last for the rest of my life. Not only is she a stubborn bitch, she’s expensive too. Please help if you can. I know I have a lot of listeners and followers who are financially comfortable. Those are the people I’m hoping will dig deep. If you’re struggling, please do as they tell you to do on a plane: Take care of yourself first. Once you’re set, then you can help those around you.
Until next time, Fuck Cancer!